Diversity in Breast Cancer — a Disease That Doesn’t Discriminate
Article
Clinical


According to the Centers for Disease Control (CDC), for non-Hispanic Black women and Hispanic women, breast cancer is the leading cause of cancer death. This article features one young woman’s heroic battle, and medical professionals going above and beyond to educate and support patients.
It should come as no surprise that Janique (Rivera) McGriff is in the law enforcement field, is a certified firearms instructor, and is an armorer (someone who knows how to fully assemble, disassemble, repair, and maintain a firearm). At age 36 and a three-time cancer survivor, you could say she’s as tough as armor and has dodged several bullets. Even her email address, which includes “pinksurvivor,” reflects her positive outlook.
 Janique McGriff
Janique McGriff
In 2017, Janique’s world started to turn upside down. “I felt a lump in my right breast on the side,” she says. “It was just the side. It was a very small lump so I didn't pay much attention to it. As months went on, it kind of got larger and it started moving towards the breast.”
The first time Janique got it checked out at the hospital, she was told that since she didn’t have any symptoms, it was likely a cyst. No mammogram or other tests were ordered. “I've had cysts before,” she says, “I kind of just like let it go. But then months went on … and it got larger and it got so big to the point where it started to lift my breast and then it became painful. So I went to my OB-GYN.”
Her doctor examined her, and she was again told it didn’t feel like it was anything other than a cyst. Janique told him it was “super painful” and asked for a referral to get it drained. So he referred her to get a mammogram at the Helen F. Graham Cancer Center & Research Institute in Delaware, where she lives.
By then it was January 2018. Upon arrival at the center, Janique was asked why she was there and she said for a mammogram. She was told she’s too young. “I do feel like age played a huge factor. No one took me seriously,” she says.
“At that point, I was kind of aggravated. … I kind of went off” she says, refusing to leave until she was tested. She was told to calm down, but ultimately got a mammogram and then an ultrasound. During the ultrasound, the tech told her she’d like to seek a doctor’s opinion. She had a biopsy the very same day.
A couple days later, Janique got a call at work and was told — over the phone — that she had cancer. “It kind of didn't hit me,” she says. When she called her mother to give her the news, her mother was very upset “because that's not how it was supposed to happen.” When Janique did go in to the doctor’s office, she was diagnosed with a very aggressive form of triple negative breast cancer (TNBC), a type that disproportionately affects African-American women. She received her diagnosis on Jan. 19, which happens to be her brother's birthday. By that time, the mass had grown to around 4 to 6 centimeters, classifying it as stage 2–3.
Like Citeline employee Claudia Maucieri, Janique was young when she was diagnosed with breast cancer — only 29. At the time of her diagnosis, Janique was married with two young children. She divorced her husband a year later and temporarily moved in with her parents. She remarried in 2022; her wife brought another daughter, now 4, via intrauterine insemination (IUI) into the family.
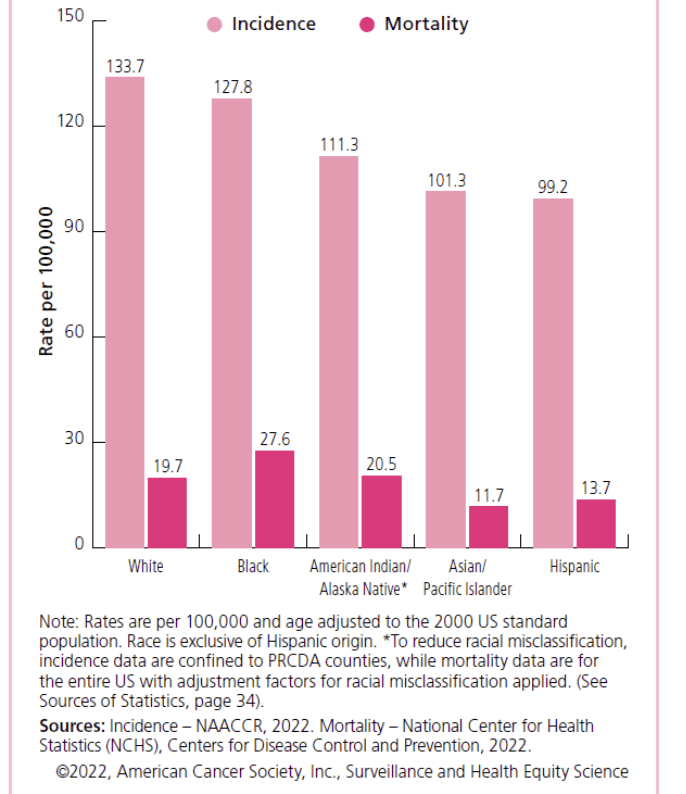
According to the Centers for Disease Control (CDC), for non-Hispanic Black women and Hispanic women, breast cancer is the leading cause of cancer death. Breast cancer is the most commonly diagnosed cancer among Black women.1 Janique is of Jamaican, Asian, and Puerto Rican descent.
Female Breast Cancer Incidence (2015–2019)
and Death (2016–19) Rates by Ethnicity, US
Janique’s aggressive cancer required an aggressive approach. “I received every scan possible,” she says, including CAT scans and MRIs. Chemotherapy was started immediately. “Within a couple weeks I had a port in,” she recalls. “I had every symptom you could possibly think of.” She went bald, her fingernails turned black, and she was nauseous. That went on for a couple of months; her tumor began to shrink, so she was switched to a less toxic drug. But she felt the tumor growing, and when she shared this with her oncologist, they told her she was overreacting, that she had to give the medicine time to work.
Again, Janique stood her ground, saying she would deny further treatment until they looked at the tumor. After undergoing a scan, the oncologist apologized and stopped the chemo. This was August 2018. A month later, Janique had a full mastectomy (her choice) of her right breast and began radiation treatments a few months later.
Following the radiation treatment, she was given the option for additional immunotherapy or to be placed in a six-week clinical trial of a drug to prevent recurrence and increase life expectancy. Janique chose the latter and was accepted. “I was a bit optimistic because I wanted to do anything possible to make my odds better,” she says. A few months after the trial, Janique had breast reconstruction surgery, including a breast implant.
Fast forward to 2020, in the midst of the pandemic. “I had just a small little cough. I thought it was the changing of the season type, like a clearing your throat.” On Valentine’s Day, she woke up with a cramp in her side.
Janique went to her job at the police department, and a half hour into her shift “it was so painful when I breathed in and out like something stabbing me in the back of my ribs. I was literally at the point of screaming. And holding my breath.” Working at the police department has its perks; she was taken straight to the hospital in a police car and was escorted right in.
She had a CAT scan, received medication for pain, and “literally within an hour they came back and said, ‘You have an 11-by-17-by-14-centimeter mass in your lung.’ Boom. Drops mic.” The reason she was in such pain was because the tumor sat on a nerve. She had no other symptoms, so without that pain the tumor would have gone undetected. Further testing revealed it was likely her breast cancer had spread. Janique says she was surprised because all her lymph nodes had tested negative. Now she was dealing with stage 4 metastatic breast cancer.
Janique underwent chemo every other week until August. Her tumor shrunk down to about 4 to 6 centimeters, so she underwent surgery the next month. The surgery was expected to take around four hours. It lasted nine. During that entire time, they provided only a single update to her mother, who was sitting anxiously in the waiting room. Janique explains that the surgeons could not access the tumor without damaging her breast implant, so they had to go around it, cutting her from the armpit down and removing a rib in the process.
After a couple months of recovery, Janique returned to work in the police force mid-November. She had lost a lot of weight and wearing full police gear — a 15-pound belt, 6-pound vest, plus the uniform — would have been too taxing. “Fortunately,” Janique says, “due to COVID, everything was shut down.” So her chief helped rotate her schedule to online work.
In mid-December, Janique began having headaches. “I was working out at the gym,” she says, “so I figured maybe I was doing a little too much.” She was taking pain relievers, but at work she told the police chief it was beginning to affect her vision and, knowing her medical history, he told her to go to the hospital. By the time she got there, her vision was almost completely blurred. A CAT scan revealed a 5-centimeter mass on her brain.
“The third one kind of took my spirit,” Janique admits. However, she knew that, for her children’s sake, “I don’t have a choice. You’ve got to get through this. You’ve got to do it.”
This time, Janique did not undergo chemotherapy. “They just went right in and cut the skull and took the tumor out,” she says matter-of-factly. This was followed by three days of non-invasive CyberKnife radiation therapy. Janique has been on immunotherapy since 2020; one treatment she was on is no longer approved by the US Food and Drug Administration (FDA). She now is on a maintenance regimen of Keytruda every six weeks. The only drawback is that it has impacted her immune system, making her so allergic that she had to give away her dog.
To date, Janique has not received results from the clinical trial in which she participated. She does not know if she received the actual drug being tested, which has since been approved, or a placebo. Based on her cancer’s recurrence, she could have received either the placebo or received the drug but it proved ineffective.
“My biggest message throughout my entire journey is definitely advocacy,” Janique says. “Every individual is not a statistic and we know our bodies better than anyone. So listen to your body and 100% advocate for yourself, because the doctor is supposed to work for you.”
Janique’s story is featured in “A Letter to My Sisters: A Breast Cancer Documentary for Young Women,” a documentary about a trio of young women dealing with their breast cancer diagnoses, written and created by radiation therapist Nia Imani Bailey.
Bailey shares her inspiration for the film, which premiered October 2022. She says that in her day-to-day job, “I saw so many young women coming in for breast cancer treatment. I met a lot of young women who looked just like me.” One of those young women was Jaclynn Smith, a patient who became a friend of Bailey’s and lost her battle with breast cancer at age 33.
In addition to Janique, the film features Brenda Durante, a Mexican woman diagnosed in her 30s, and Lynne Mitchell, of German-Irish-Swedish descent, diagnosed with triple negative breast cancer in her 40s. “I wanted to get a diverse pool of women, diverse ages,” so that all women could identify with them, Bailey explains.
In November 2023, Bailey founded the Byrd Cancer Foundation, whose mission is to “assist individuals battling cancer by connecting them to support and resources.” In addition, Bailey says the foundation’s goals are to teach people, patients, and the community how to prevent, treat, and survive cancer. Resource referrals range from integrative therapies, counseling, and nutrition to house cleaning and paying bills.
To coincide with Breast Cancer Awareness Month, the foundation has partnered with NOWINCLUDED to amplify breast cancer awareness and education. They are releasing a series of educational videos featuring stories from breast cancer survivors, including a male breast cancer survivor who identifies as gay and individuals from various cultural and linguistic backgrounds. These videos are available in Spanish, French, Tagalog, and Polish.
The campaign seeks to engage underrepresented communities in breast cancer discussions, including men and non-English-speaking populations. The partnership will also spotlight unique survivor journeys, including individuals with dense breast tissue or those diagnosed with breast cancer during pregnancy.
As of Sept. 10, 2024, the FDA requires that all mammogram reports sent to patients must include breast density, which should be described as either “not dense” or “dense.” It’s a triple whammy: Women with dense breast tissue — about 40% of all women — have a higher risk of breast cancer, Black women have 21% to 31% greater breast density compared to their white counterparts, and dense breast tissue also makes it harder for radiologists to see cancer on mammograms. For more information, visit DenseBreast-info.org.
 Dr. Nia Imani Bailey
Dr. Nia Imani Bailey
A patient herself, navigating the complexities of the healthcare system with lupus and carrying a cancer gene, Bailey brings firsthand knowledge to her advocacy work, creating a synergy between her roles as a healthcare professional and a patient. “It’s no surprise that women always get dismissed. We’re second class,” she says.
“I think there still needs to be physician education. … Women are strong, but that doesn’t mean you can dismiss when a woman is in pain or says ‘Something is wrong with my body.’ Listen to your patient.” Bailey also suggests her physician colleagues do more to avoid discrimination in healthcare. “Check your biases at the door,” she advises.
Her advocacy work includes serving as an adviser for the Bexa Equity Alliance, as a member of the Unite for HER Women of Color Task Force, and as a board member of the Still Rise Farm Organization.
 Dr. Monique Gary
Dr. Monique Gary
Breast surgeon and oncologist Monique Gary, known to her patients as “Dr. Mo,” serves as medical adviser for the Byrd Foundation. In this role, she leverages her expertise to support its initiatives and help advance cancer care for all communities.
She is Medical Director of the Grand View Health/Penn Cancer Network cancer program, where she also serves as director of the breast program, and an adjunct associate professor at Dartmouth College. Gary has been recognized as a Leading Physicians of the World and Top Breast Surgeon in Pennsylvania for 2017, 2018, and 2019.
When asked why she chose to specialize in breast surgery/oncology, Gary says, “I think it’s fair to say that this career path chose me. When I was 7 years old, my mother was diagnosed with ovarian cancer, and she died within a year. She was 29, with two girls, and all we knew at the time was that our mom was really sick. Then we started to hear the word ‘cancer’ being whispered. When I was about 12, my grandmother got breast cancer. Doctors tried to tell my grandma she had six months to live, and I watched as my grandmother advocated for herself, refusing to accept the doctor’s prognosis. Fifteen years later, she was diagnosed with breast cancer in her other breast. Again, I watched as my grandmother advocated for herself and gained support from the community. My grandmother went against the odds and outlived the 6- to 12-month expectancy the doctors gave her, and ultimately died 25 years later. I look back, and this was my first real example of self-advocacy.”
She is a vocal advocate for diversity and improving trust in clinical trials, including this BlackDoctor.org town hall on the importance of real-world data (RWD) in trials, particularly for the Black community. In this article, she shares her perspective on diverse patient enrollment. “Diverse representation in clinical research matters,” Gary says, “and we need a new framework, powered by a multi-stakeholder consensus, to move the needle of our biggest research challenge as it relates to health parity.”
Gary is CEO of Still Rise Farms, a 40- acre farm that was founded as a wellness incubator for cancer patients and under-resourced, marginalized communities. She recently hosted her fifth biannual retreat for about 50 women, patients and survivors of breast (whom Gary calls “breasties”), cervical, uterine, and ovarian cancers. An article in The Philadelphia Inquirer gives a behind-the-scenes look at the retreat and its positive impact on attendees.
Promoting healthy living and cancer risk reduction, Gary also can be found on radioOne stations in Philadelphia, and weekly on Blackdoctor.org as the co-host of “The Doctor Is In,” a web series dedicated to promoting survivorship in breast cancer patients and arming them with both science and support.
“People don’t care how much you know until they know how much you care.”
Gary was an adviser for Novartis’s More Than Just Words initiative, created to provide resources, systems, and community for Black women to increase health equity in breast cancer care. Currently an ambassador for the project, she supports initiatives focused on augmented reality health tools and training for clinicians, as well as advancing community advocacy and improving health literacy.
She currently serves as the professor for national breast cancer advocacy organizations, including Living Beyond Breast Cancer, TOUCH (The Black Breast Cancer Alliance), Tigerlily Foundation, The Chrysalis Initiative, and the National LGBT Cancer Network.
“Every day, in addition to treating cancer,” Gary says, “I am shattering expectations and stereotypes of who and what Black women can be and do, both in medicine and in leadership, and research and industry.”

Darcy Grabenstein
Director of Content Strategy and Thought Leadership | Citeline
Darcy is the Director of Content Strategy and Thought Leadership for Citeline. A journalist by training, she has more than 30 years of experience in marketing, advertising, and public relations.